
Beyond HbA1c: A more complete picture with structured blood glucose monitoring
Although HbA1c measurements are the traditional measurement for assessing the effectiveness of diabetes management, and are valuable as a long-term glycaemic marker, HbA1c does not provide insight into short-term glycaemic exposure, or episodes of high or low blood glucose that patients experience1. In order to gain a more complete picture, HbA1c should be combined with structured self-monitoring of blood glucose (SMBG).
As a stand-alone value, HbA1c does not provide information about specific times your patient experienced variations in their blood glucose levels, or what may have prompted these variations. Relying solely on this measurement can therefore be deceiving, and can fail to reveal2,3:
- Glycaemic variability
- Episodes of acute hypo or hyperglycaemia
- Differing glycation rates between patients
- Elevated fasting glucose levels
- Postprandial hyperglycaemia
Structured SMBG gives you a more complete picture of when and why your patient experiences glucose fluctuations. A structured SMBG monitoring regimen can identify patterns in glycaemic changes, as well as reveal what behaviours could be driving those shifts (e.g. medications, exercise, food). SMBG offers different types of structured monitoring, depending on the need.
Choose a structured monitoring plan based on the need
For on-going, longer-term evaluation of glucose-impacting factors, consider individualised monitoring:
- Insulin management monitoring to assess the impact of a change in medication or insulin doses on blood glucose levels, or to monitor a patient’s transition to a new therapy
- Lifestyle intervention monitoring to demonstrate the impact of a change in diet, exercise, or other glucose-impacting behaviours on blood glucose management
For episodic, short-term SMBG monitoring, focused checks are recommended to support the treatment of non-insulin-treated patients with type 2 diabetes who4:
- Have signs of hypoglycaemia risk
- Experience worsening HbA1c values
- Experience illness, elevated stress levels, or travel
- Are undergoing changes to medication, diet, or physical activity
- Undergo a significant life change, such as starting a new job or moving house
- Need additional information about the state of their disease or the impact of their treatment plan on glycaemic management
- Are pregnant or planning pregnancy
Insight to hyperglycaemia and glycaemic variability
The data collected from structured SMBG monitoring gives patients a broader understanding of how their behaviours and decisions directly impact their diabetes and blood glucose levels.
HbA1c can also be misleading about glycaemic variability - the degree of fluctuations people with diabetes experience between low and high blood glucose levels. Because it is an average calculated over multiple months, two people can have the same value but wildly different fluctuations6.
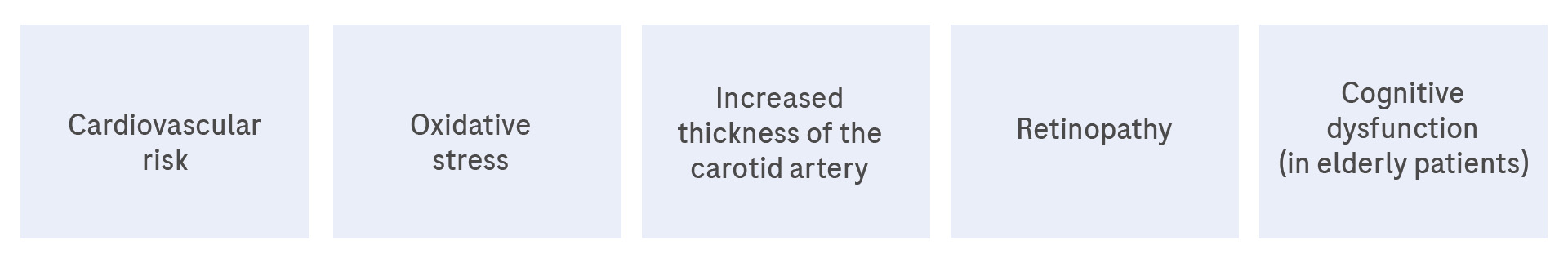
Glycaemic variability, specifically when related to postprandial hyperglycaemia, has been associated with an increased risk of complications. Complications that can arise from postprandial hyperglycaemia (see figure 1) or glycaemic variability include5:
- Macrovascular disease (independent of HbA1c)
- Cardiovascular disease
- Oxidative stress
- Endothelial dysfunction
- Atherosclerosis
There is a body of evidence that shows that there is a benefit to blood glucose monitoring in people with type 2 diabetes, providing it is structured8,9,10.
Consistently using SMBG to monitor your patient’s diabetes can contextualise out-of-target glucose levels with factors such as activity, food, stress, illness, and medication. Accu-Chek tools and resources can help you introduce structured testing activities to your patients in manageable, collaborative steps. Check out our downloadable patient tools:
- The Accu-Chek® Testing in Pairs tool – a simple “before and after” even testing plan
- The Accu-Chek® 360° View Tool – for a comprehensive 3-day, 7-point glucose profile
References:
1. Dailey G. Assessing glycemic control with self-monitoring of blood glucose and hemoglobin A1c measurements. Mayo Clin Proc. 2007;82(2):229-36.
2. Hinzmann R, et al. What Do We Need beyond Hemoglobin A1c to Get the Complete Picture of Glycemia in People with Diabetes? Int J Med Sci. 2012;9(8):665-81.
3. Polonsky WH, Jelsovsky A, Panzer S, Parkin CG, Wagner RS. Primary care physicians identify and act upon glycemic abnormalities found in structured, episodic blood glucose monitoring data from non-insulin treated type 2 diabetes. Diabetes Technol Ther. 2009;11(5):283-91.
4. International Diabetes Federation Clinical Guidelines Taskforce and SMBG International Working Group. Self-monitoring of blood glucose in non-insulin-treated type 2 diabetes. Brussels: International Diabetes Federation. 2009.
5. American Diabetes Association. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2021. Diabetes care. 2021;44(Suppl 1):S15–33. https://doi.org/10.2337/dc21-S002.
6. Leiter LA, Ceriello A, Davidson JA, Hanefeld M, Monnier L, Owens DR, Tajima N, Tuomilehto J, for the International Prandial Glucose Regulation (PGR) Study Group. Postprandial glucose regulation: new data and new implications. Clin Ther. 2005;27(Suppl B):S42-56.
7. International Diabetes Federation. Guideline for Management of PostMeal Glucose in Diabetes. 2011.
8. Parsons SN, Luzio SD, Harvey JN, et al. Effect of structured self-monitoring of blood glucose, with and without additional TeleCare support, on overall glycaemic control in non-insulin treated Type 2 diabetes: the SMBG Study, a 12-month randomized controlled trial. Diabet Med. 2019;36(5):578-590. doi:10.1111/dme.13899
9. Polonsky WH, Fisher L, Schikman CH, et al. Structured self-monitoring of blood glucose significantly reduces A1C levels in poorly controlled, noninsulin-treated type 2 diabetes: results from the Structured Testing Program study. Diabetes Care. 2011;34(2):262-267. doi:10.2337/dc10-1732
10. Chircop J, Sheffield D, Kotera Y. Systematic Review of Self-Monitoring of Blood Glucose in Patients With Type 2 Diabetes, Nursing Research: 11/12 2021 - Volume 70 - Issue 6 - p 487-497
doi: 10.1097/NNR.0000000000000542